Introduction
Sports practice is promoted as a means for health improvement in general. However, it ought to be taken into account that, when inappropriately or excessively practiced, it may lead to undesired secondary effects1.
In fact, it is generally accepted that, in elite athletes, sports practice may be more detrimental than beneficial, provoking multisystemic damage such as muscular, osteoarticular, cardiac, etc.2-6. In line with this, reproductive function has been assessed in athletes with regards to possible negative effects. Due to clear symptoms (delayed menarche, amenorrhea, oligomenorrhea), researchers postulated the existence of a relationship between exercise and reproductive function in female athletes7-13.
Such relationship has been harder to assess in male athletes due to the absence of symptoms as evident as in the case of female athletes. However, many researchers have tried to assess this relationship by means of hormonal and/or seminological evaluations14-18. De Souza and colleagues established that, in order to observe alterations in semen parameters, a minimum effective volume of a 100 km/week had to be attained17,18. We have also observed, when comparing different exercise modalities, that triathletes had worse values for seminological parameters than physically active subjects and/or water polo players19. In fact, one of the parameters that seemed to be more affected by exercise load was sperm morphology. Sperm morphology is an essential parameter in the assessment of male fertility20-23. This parameter can offer an estimation of the prognosis for in vivo and in vitro conceptions22,23, and it may be, by itself, the most important parameter in the assessment of male.
It is known that triathlon is one of the sports with the highest training volume, which was also observed in our previous study19. We hypothesize that sperm morphology is more susceptible to alterations due to sports practice, especially high volume training. Thus, the aim of the present study was to correlate, in international level triathletes, the weekly volume covered as part of their regular training to the percentage of sperm exhibiting normal morphology (sperm morphology).
Methods
Subjects
Fifteen male subjects participated from the present study. The study was approved by the Institutional Review Board of the University of Córdoba, and informed consent was obtained from all participants. The participants composed a rather homogenous sample, they were aged 33.1 ± 3.5, and had a weight (kg), height (cm), and body fat (%) of 74.5 ± 7.6, 175.3 ± 3.7, and 7.0 ± 2.9, respectively. As for their exercise background, it should be noted that they had been practicing for several years, as it would be expected from the level in which they were competing. The subjects, with a VO2max of 64.0 ± 5.1 ml/min/kg, had been training for 8.1 ± 3.2 years.
In order to rule out any possible factors affecting sperm production (childhood illnesses, trauma, surgery, etc.), a physician reviewed the subjects' medical histories as well as intake habits (alcohol, cigarettes, coffee, etc.) and occupational risks, which were assessed by means of specific questionnaires.
Any subject that could present with an impaired reproductive function due to factors other than exercise was excluded from the study. Not having any exclusion criteria, and having participated, and finished, in the Ironman competition were considered as inclusion criteria for the study. Training was carefully assessed in detail, especially regarding weekly volume expressed both as total volume and as volume for each of the modalities.
Procedures
With regards to weekly volume, an assessment of the training periodization was performed, and all subjects answered a questionnaire about their weekly training, stating the volume, both in time (minutes), and in covered distance (km) for every one of the modalities trained, that is, running, cycling and swimming. This information was used for the analysis of weekly training volume as well as for subsequent correlation studies with sperm morphology.
As for morphology assessment, subjects collected, into a sterile container, the semen sample after a period of abstinence of 3-6 days. For proper sperm morphology assessment and categorization, Kruger's strict criteria were followed24. For such purpose the participants were required to bring the sample to the lab within 30 minutes after collection. Two slides of sperm extensions were prepared for each subject. The sperm extensions were stained using a quick stain (Diff Quick, Dade Diagnostics, Fla. USA). Two-hundred sperm per subject were analyzed with the 100x under oil, observing and recording any abnormalities. Head, midpiece, and tail were assessed for each spermatozoon. Any borderline form was considered abnormal according to Kruger's guidelines.
Statistical analysis
One-way ANOVA was performed to compare weekly volumes (minutes, and distance) among the practiced modalities. Data normality was assessed through the Shapiro-Wilk test and standard visual inspection; all variables (cycling volume, and sperm morphology) presented normal distribution. Pearson correlation studies were performed to verify relation between cycling km/week and sperm morphology. Statistical significance was set at p < 0.05 and values were given as mean ± standard deviation.
Results
The assessment of training periodization and the applied questionnaire revealed the following values with regards to training: 9.9 ± 1.8 sessions per week, and 122.6 ± 62.7 minutes per session.
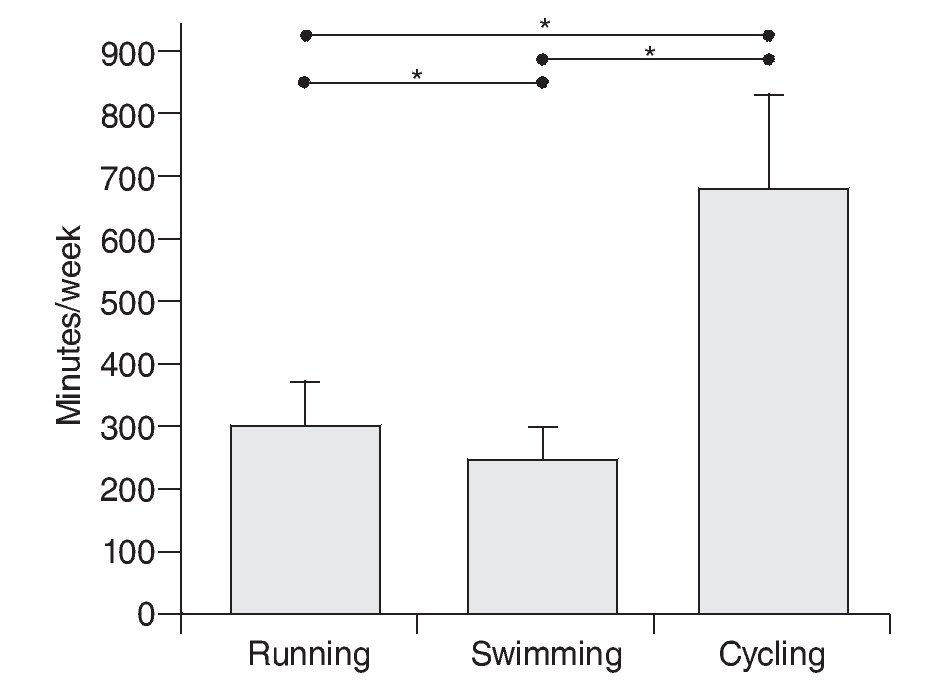
Figure 1 shows the volume distribution triathletes undergo for running, swimming, and cycling, expressed as total weekly minutes. It can be observed how the triathletes spend significantly more time for the cycling modality than any of the other two (p < 0.05). Triathletes, as it can be derived from the figure 1, spend less time training for the swimming modality (p < 0.05).
Fig. 1. Distribution of weekly training volume per practiced modality (expressed as minutes/week). Total volume= 1,204 minutes/week. *Significantly differences (p < 0.05) between modalities.
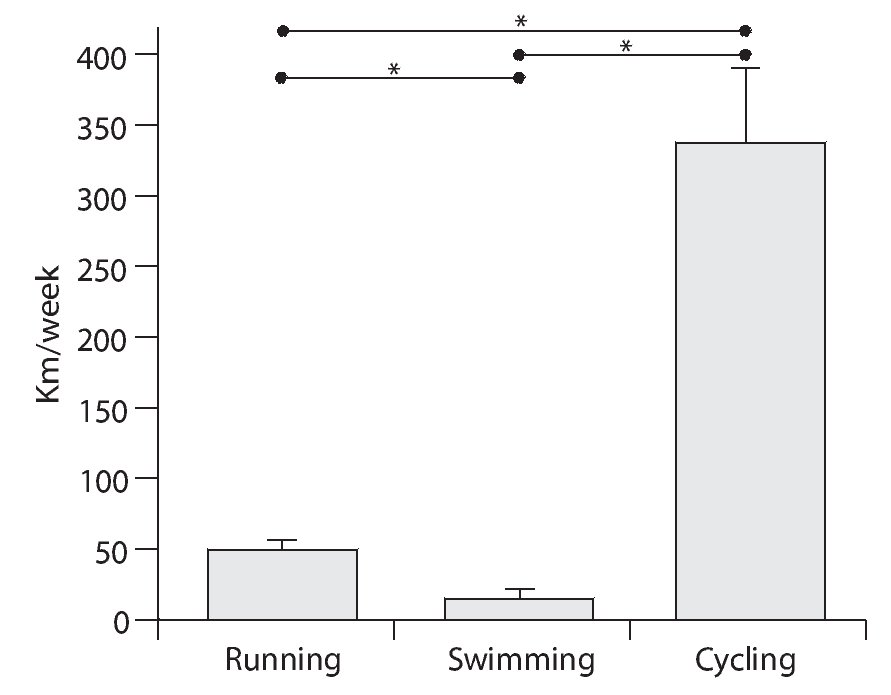
Moreover, it can be observed how the differences among the three modalities increase if, instead of considering the time employed in each modality, the total volume expressed as kilometres/week is analyzed. As it would be easily expected from the time employed, triathletes cover a greater distance in the cycling modality than in any of the other two modalities (fig. 2).
Fig. 2. Distribution of weekly training volume per practiced modality (expressed as km/week). Total volume = 391.5 km/week. *Significantly differences (p < 0.05) between modalities.
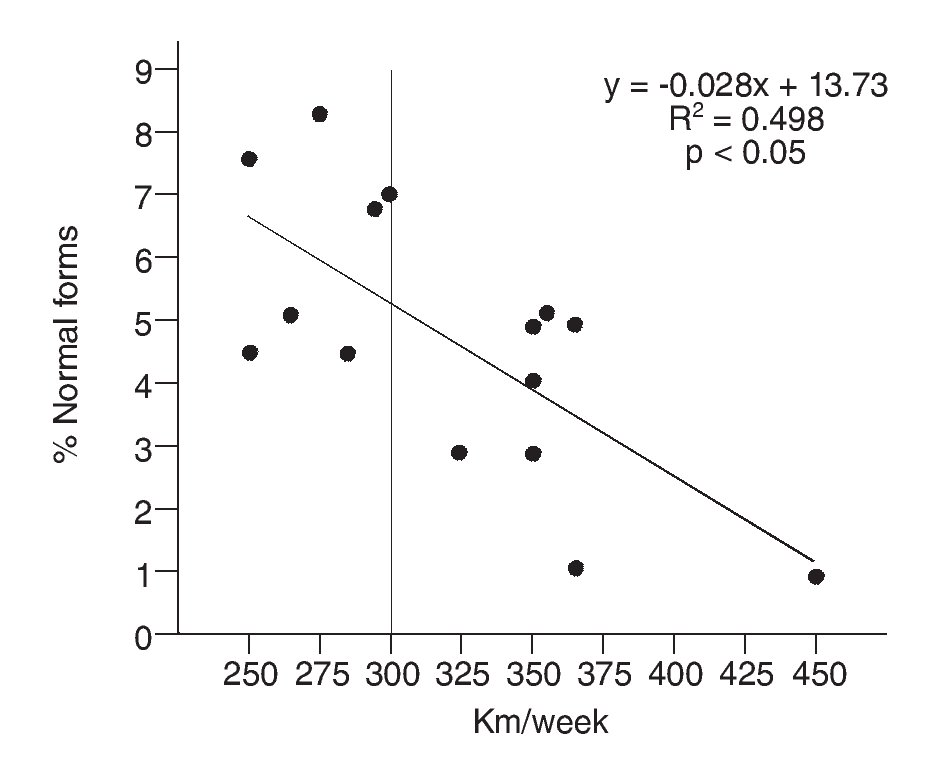
When analyzing the correlation between the number of covered kilometers and the number of normal forms, total weekly volume did not show any correlation (r = -0.29; p > 0.05). Neither running nor swimming showed any correlation either (r = -0.12; p > 0.05; r = 0.09; p > 0.05, respectively). Cycling modality, however, showed a high inverse correlation (r = -0.71; p < 0.05) between the distance covered and the number of normal sperm forms (fig. 3).
Fig. 3. Correlation between percentage of sperm with normal morphology and cycling weekly volume (expressed as Km/week).
Discussion
The main finding of the present study is that cycling training volume inversely correlates to sperm morphology. That is, athletes with the highest weekly training volume (greatest distance covered in km) had the lowest percentage of normal sperm.
Besides being common knowledge, we undertook a careful observation and analysis of the volume triathletes practice in each modality. If we take in consideration that while running volume, swimming volume, and total volume did not show significant correlation with sperm morphology, the high correlation observed for the cycling modality may rely on factors inherent to cycling modality besides the covered volume.
Since cycling was the modality with the greatest volume, it seemed logical that this modality would be the one with the greatest possibility for producing anomalies in sperm production. Moreover, as derived from the fact that total volume did not significantly correlate to sperm morphology, cycling might be the most detrimental modality not only for volume reasons but also for factors inherent to cycling training (saddle, clothing, etc.). While all subjects have a value for sperm morphology below 14% which is the traditionally accepted value for normality according to Kruger's strict criteria, those with higher training volume in cycling have lower values than the other subjects. Moreover, it seems that those systematically covering distances over 300 km per week (fig. 3) would have values so low that they would be included in the p-group (poor prognosis) with regards to pregnancy outcome according to Kruger's newest categorization25,26. It would be expected, therefore, that subjects in this category would have problems when trying to conceive.
Our results seem to be in agreement with those previously published by other groups17,18,27. It seems that the volume threshold hypothesis may be confirmed. This study not only seems to confirm such hypothesis but also adds substantial information so as to how affected sperm are.
Sperm morphology seemed the most altered parameter as derived from previous studies27-29. Due to the importance of morphology, and its apparent susceptibility, it became, therefore, the aim of the correlation in the present study.De Souza and colleagues established 100 km week-1 as the threshold value for sperm abnormalities17,18. They established this threshold for the running modality. While our subjects had not undergone such running volume, they had a higher volume both in cycling alone and for the combination of the three modalities. In any case, it is deemed possible that each modality may have its own volume threshold, especially since metabolic requirements are expected to be different. In fact, as Gebreegziagher and colleagues27 suggests, the different effects produced on spermatogenesis by different modes of exercise may be due to different stress factors imposed on the body, such as physical, chemical, and biological. Endurance exercise is generally accepted to be able to produce changes in body temperature and hormonal milieu. This condition may be further aggravated in cycling where subjects are clearly exposed to mechanical compression and irritation, even sometimes producing a microtrauma, of the testes, epididymis, and vas deferens during cycling27,28. Due to such compression, a reduction in blood flow may occur; this aspect is of special importance since nutrition of the sperm cell line-ages may be impaired.
The compression of the area, produced mainly by the bike saddle and the tight culottes worn, may generate an undesired increase in intrascrotral temperature which is well known to be detrimental for the sperm production process, especially causing interference in the development of primary spermatocytes30,31. Reduction in testosterone levels due to prolonged bouts of exercise has also been reported; this, obviously, could seriously compromise spermatogenesis32. Moreover, changes in body mass and energy balance, which may be modality specific, may also play a role in the appearance of male reproductive pathology. Thus, the effect of different modes of exercise on spermatogenesis may differ. On the other hand, from the obtained results, it seems evident that exercise-related infertility problems are not only observed among different modalities but also within the same modality.
For triathletes, it is difficult to estimate what the volume threshold would be to start observing alterations, especially since they all undergo high volumes. However, it can be concluded that a high cycling volume is detrimental to sperm morphology. Moreover, it can also be inferred that a distance of 300 km/week seems to be the threshold in cycling for a serious impairment in fertility.
Future research is needed to further clarify the relationship between training volume and male fertility-related problems, and maybe even determining volume thresholds that can be modality-specific. Studies should be undertaken to assess sperm morphology in more detail and try to find out what the mechanism behind these alterations is.
Correspondence:
D. Vaamonde.
Morphological Sciences Department.
School of Medicine. Universidad de Córdoba. Avda. Menéndez Pidal s/n.
14071 Córdoba. Spain.
E-mail:
fivresearch@yahoo.com
History of the article:
Received January 16, 2009
Accepted March 30, 2009 ONT>Received January 16, 2009
Accepted March 30, 2009